The continuing stress on health care workers, a possible employee mass exodus at the end of the pandemic, and veterans delaying needed health care could combine to create even more of a strain on the Veterans Administration health care system after the pandemic ends, said the official in charge of that system.
“The workforce is tired, and they’re mentally exhausted….. I have very significant concerns that on the other end of this, we will see significant retirements that’s going to challenge us,” said Dr. Richard Stone, executive in charge of the Veterans Health Administration, during a session at the annual meeting of the Association of Military Surgeons of the United States Wednesday.
“Sometime in late 2021, we may see large numbers of people retiring. How do we maintain this very skilled, very mature workforce that represents the VA employee?”
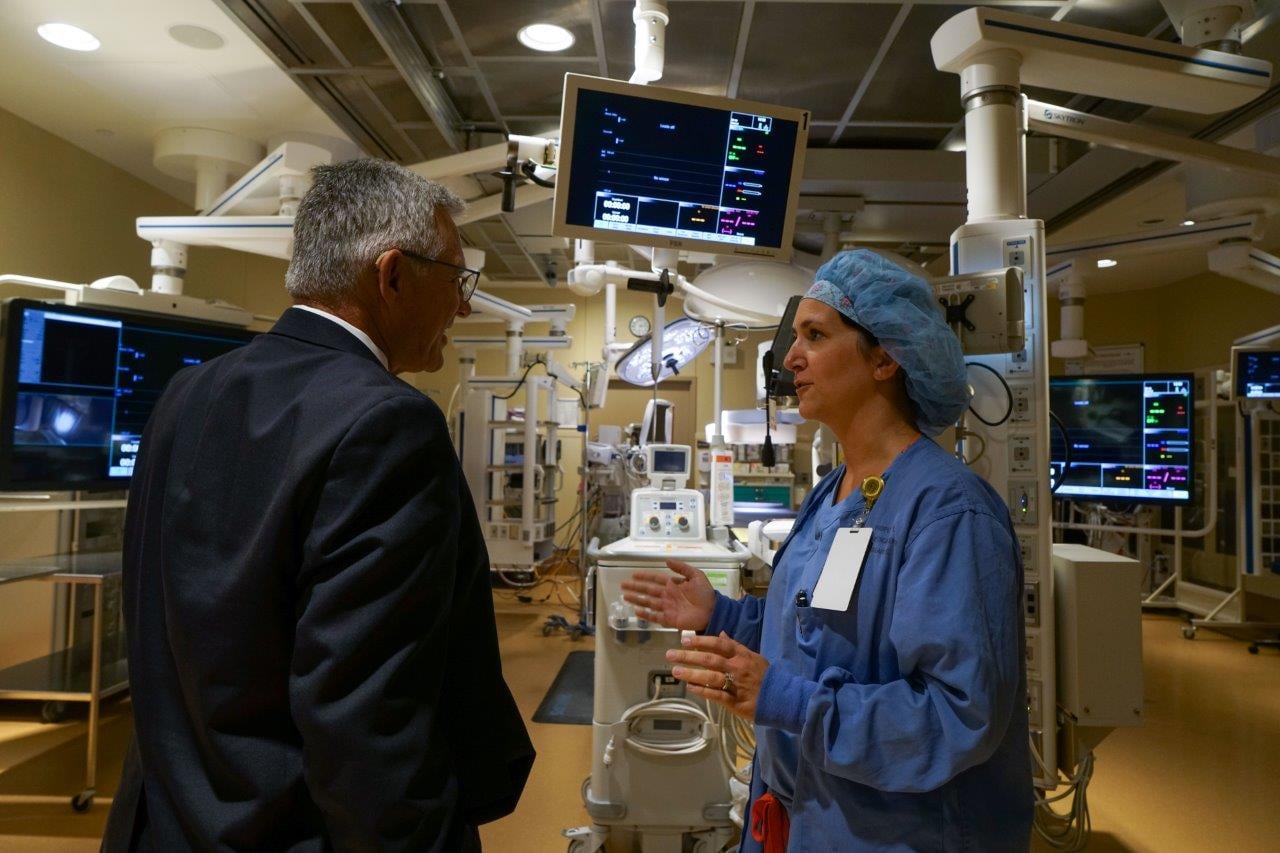
Stone said he has personally seen the signs of stress and burnout in the faces of personnel in VA medical facilities, and said he’s reassuring employees that VHA is continuing to hire more personnel. Since March, VHA has hired 60,000 employees, and increased its nursing ranks by 11,000. The Office of Personnel Management has supported VA’s efforts by drastically reducing the hiring time — from 100 days in some places, to less than 20 days, Stone said. But it’s getting harder to hire medical personnel, as the pool of employees is drying up, he said.
Stone is also concerned about the inability of employees to take leave and recharge — which many employees especially do around the holidays. As the holidays approach, the COVID cases are increasing.
As of Tuesday evening, VA health officials at 140 sites across the country were tracking nearly 17,000 active coronavirus cases among patients and staff. That total is an increase of more than 400 percent since Oct. 1.
At least 5,443 VA patients and 77 VA employees have died from complications related to the virus in the last nine months. Doses of the coronavirus vaccine are expected to be shipped to an initial 37 VA medical sites over the coming days, but plans for distribution remain unclear.
More problems are over the horizon after the pandemic ends.
There are concerns about delayed health care, he said. The VHA is now performing about 86 percent of the surgeries they did before the pandemic, he said, and there’s a buildup of surgeries that need to be done. He thinks it will take three to six months to work through the backlog.
Delays in screening tests, such as endoscopy and mammograms, could also have long term effects.
“We think the buildup of delayed diagnoses may result in very significant risk to the American population,” Stone said. “We have been pushing really hard to get people in for screening mammograms, and we’re beginning to see recovery of those numbers. In many areas of the country we are seeing large numbers coming in for screening tests. But we have a pretty good built-up backlog we need to resolve,” he said.
At the beginning of the pandemic, VA providers canceled about 6 million appointments, Stone said, and since then, providers have had interactions with about 90 percent of those veterans, to make sure there aren’t delays in necessary care. Unfortunately, there are a lot of patients who still believe it’s unsafe to come in, he said, and primary care providers have worked hard to convince these patients, he said.
RELATED

These are problems many medical facilities across the country are facing. U.S. Surgeon General Vice Adm. Jerome Adams, of the U.S. Public Health Service, said the country needs to think about what the health care transition will look like as the pandemic ends, and how health care providers will encourage people to come in for their health care needs.
“I’m convinced that even if we end the pandemic in 2021, we’re going to see the losses for years, maybe decades to come, in the way of missed diagnoses,” he said, during the session at AMSUS where he talked with Stone.
Adams described the situation of his wife, who is undergoing cancer treatment. A screening she was supposed to have at the beginning of the pandemic was pushed back several months, delaying the diagnosis.
“We will never know if it will ultimately have an impact on her outcome,” Adams said. “I’ve personally experienced some of the negative harms that are indirectly related to COVID-19.”
In this third surge of COVID, he said, “we need to do all we can to preserve preventive care,” given the situation is different now than at the beginning of COVID, when the country faced shortages of personal protective equipment, concerns about capacity, and other issues.
Stone said they’ve tried to maintain a large amount of outpatient care in VA, “but this third wave has been so robust across the nation, that it’s been a challenge.” With the current sure in coronavirus cases, “there are some areas so substantially stressed for inpatient personnel that we’ve had to shut down parts of our ambulatory care system,” Stone said. Ambulatory care is medical care provided on an outpatient basis.
Stone is not just concerned about the mental health of his staff, but about the mental health of veterans.
“We as veterans don’t do as well when we’re isolated,” he said. While they haven’t seen increased numbers deaths by suicide as part of the pandemic, he said, they’ve seen a significant increase in the use of the veterans crisis line.
More than 80 percent of the mental health resources that VA previously provided in a face-to-face setting are now being done using telemedicine.
While he’s proud of the telemedicine resources being used across VHA, Stone said, many veterans are uncomfortable with that method when it comes to group therapy. “Veterans help veterans in group therapy,” he said.
VA health officials are encouraging employees to reach out to each other for help, and to help each other. In addition to hiring more staff, officials are taking steps such as moving personnel from some areas to help with more critical needs. They’ve trained some of those outpatient care nurses in order to bring them in to support critical care nurses within the limits of their licensure, so that those critical care nurses are not alone with multiple patients, he said.
That caregiving might mean the simple but important act of holding the hand of a critically ill patient, who may be facing death alone as families are unable to be at the bedside of their loved one.
“That has taken a huge toll on our caregivers. They’re very experienced, but it’s been emotionally gut-wrenching to get through the process of not having family members at bedside,” Stone said.
Staff writer Leo Shane contributed to this report.
Karen has covered military families, quality of life and consumer issues for Military Times for more than 30 years, and is co-author of a chapter on media coverage of military families in the book "A Battle Plan for Supporting Military Families." She previously worked for newspapers in Guam, Norfolk, Jacksonville, Fla., and Athens, Ga.