Health care providers in Veterans Health Administration facilities often failed to fully inform patients and caregivers about the risks of the COVID antiviral remdesivir in the months before the drug was approved by the Food and Drug Administration, according to a report Thursday by the Veterans Affairs watchdog.
The VA Office of Inspector General pointed to “significant deficiencies” in health care providers’ compliance with requirements to notify patients and caregivers about remdesivir’s risks, alternatives and lack of FDA approval.
The OIG interviewed VHA employees and reviewed health records of 825 patients administered remdesivir between May, when the FDA authorized the drug for emergency use, and October 2020, when the FDA approved the drug.
Of these 825 cases, according to the OIG report, health care providers failed:
- to provide 62% of patients or caregivers with a fact sheet about remdesivir
- to inform 41% that remdesivir was not FDA-approved
- to notify 32% that they had the option to refuse remdesivir
- to inform 37% of the risks and benefits of the drug
- to advise 59% of the alternatives to receiving the drug
“This could have resulted in patients or caregivers lacking the information needed to make a fully informed decision to receive the medication,” the report stated.
In interviews with the OIG, VHA leaders said they believed that providers had actually informed patients or caregivers but had not documented doing so, according to the report.
The OIG recommended that, going forward, the VHA ensure its hospitals fully inform patients about non-FDA-approved drugs. The VHA concurred with the recommendation.
Possible side effects of remdesivir include increased levels of liver enzymes, which may signify liver injury, and allergic reactions, according to the FDA.
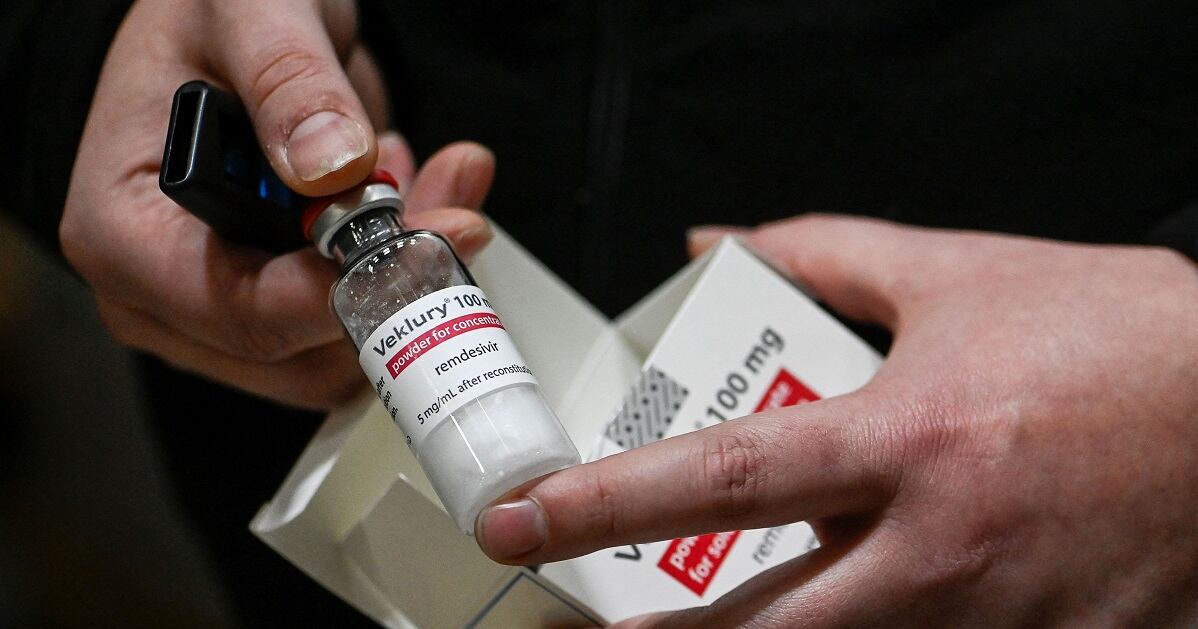
Originally developed as a possible treatment for hepatitis, remdesivir has shown mixed results in treating COVID. Some studies, including a 2022 meta-analysis, showed it reduced mortality or recovery time for patients severely ill with COVID, but other studies showed no effect.
Then-President Donald Trump took remdesivir, among other drugs, when he was treated for COVID in early October 2020.
More than 650,000 veterans connected to the Veterans Health Administration have contracted COVID-19 since the first cases were confirmed in America 31 months ago, and more than 22,000 have died from complications related to the virus.
Irene Loewenson is a staff reporter for Marine Corps Times. She joined Military Times as an editorial fellow in August 2022. She is a graduate of Williams College, where she was the editor-in-chief of the student newspaper.